When Can Medicare Supplement Insurance Plans Be Purchased
Are you looking at buying a Medigap policy? It’s a great way to cover the additional costs associated with your annual healthcare expenses.
When can Medicare supplement insurance plans be purchased? The best time to enroll in Medigap is during the six-month Medigap “Open Enrollment” period.
 This period lasts from the day of your 65th birthday or from when you take your Original Medicare Parts A & B.
This period lasts from the day of your 65th birthday or from when you take your Original Medicare Parts A & B.
Medicare has an open enrollment period from three months before your 65th birthday to three months after.
If you miss these open enrollment periods, the insurer will likely require you to undergo medical underwriting for your Medigap policy.
That means they’ll send you for an examination to assess your current healthcare status. If you have a pre-existing health condition, it might mean that your insurer charges you more for your premiums, or they might deny your application altogether.
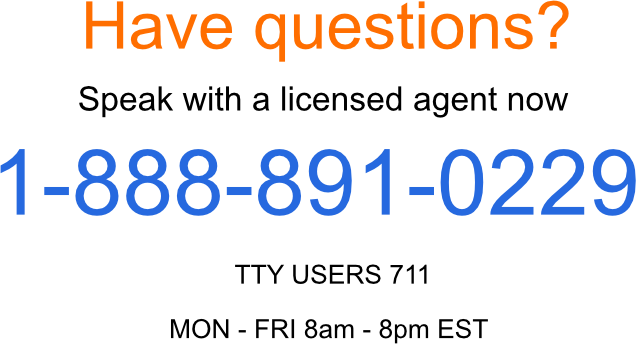
Call Us for Expert Advice in Enrolling in Medigap
If you’re unsure about when to enroll in Medigap, speak to the professionals. We offer you a free consultation on signing up for Medigap with any insurer.
Our online calculator provides a way to find the insurer with the lowest rates in your state, giving you a free automated quote on your policy.
Or you can reach us directly at 1-888-891-0229 to discuss your needs. If you can’t talk right now, that’s okay.
Complete the contact form on our site, and we’ll have a Medigap expert get in touch with you at a time that suits you.
Compare Plans & Rates
Enter Zip Code
What Does Medigap Cover?
Medigap is a supplemental insurance policy complementing your Medicare Parts A & B policies. You must have both to enroll in Medigap.
Medigap provides supplementary coverage for the following healthcare services covered or not covered by Original Medicare Parts A & B.
- Medicare Part A hospice copayments or coinsurance costs
- Medicare Part A hospital fees and coinsurance.
- Medicare Part B coinsurance or copayment costs
- blood transfusion costs up to the first 3 pints.
In addition, some Medigap plans also cover the following:
- Skilled nursing facility care costs.
- Medicare Part A deductibles.
- Medicare Part B deductibles.
- Medicare Part B excess fees.
- 80% of expenses involved in emergency medical costs during foreign travel
Can I Enroll in Medigap If I Have a Group Health Plan with My Employer or Union?
If you’re currently involved with an employer’s Medicare scheme or belong to a union. You’ll want to wait to enroll in Original Medicare Part B. Employer healthcare plans usually provide coverage similar to what you get with Medigap, so you don’t require the coverage offered by a Medigap policy.
You can enroll in Original Medicare Part B, with no penalties, when your employee coverage ends. Your open enrollment period into Medigap only starts when these befits end.
If you enroll in Part B while still using your employer’s Healthcare plan, your Part B coverage and Medigap open enrollment window start from this date.
Special Conditions for Enrolling in Medigap
If you’re under 65 and have a disability or an acute pre-existing condition like ALS or End-Stage Renal Disease (ESRD), you can’t enroll in Medicare and Medigap policies.
Typically, Federal law doesn’t require insurers to provide Medigap plans to people under 65. However, some US states provision insurers to sell Medigap to people under 65 with these health conditions.
These states are the following.
| Arkansas | Kentucky | New Jersey |
| California | Louisiana | New York |
| Colorado | Maine | North Carolina |
| Connecticut | Maryland | Oklahoma |
| Delaware | Massachusetts | Oregon |
| Florida | Michigan | Pennsylvania |
| Georgia | Minnesota | South Dakota |
| Hawaii | Mississippi | Tennessee |
| Idaho | Missouri | Texas |
| Illinois | Montana | Vermont |
| Kansas | New Hampshire | Wisconsin |
Can You Enroll in Medigap If You Have a Pre-existing Health Condition?
If you apply for a Medigap policy within the open enrollment period, the insurer cannot deny you access to its Medigap scheme.
They also can’t charge you higher premiums on your policy. They also can’t issue a waiting period with activating your benefits.
You can choose any plan from any provider and get immediate coverage for your additional medical expenses not covered by original Medicare.

So, if you have a pre-existing health condition, such as diabetes or sleep apnea, it’s best to take advantage of the open enrollment window. Register a Medigap policy as soon as possible to avoid medical underwriting.
However, the Medigap insurer may sometimes refuse to cover the out-of-pocket expenses involved with your healthcare costs if you apply outside of the open enrollment period. The waiting period can last three to six months and varies between insurers.
After completing the waiting period, the Medigap policy will cover all the treatments and care associated with your pre-existing condition. However, this isn’t always the case.
Some insurers might decide your pre-existing health status bears too much risk for the company, causing them to deny your Medigap application.
New enrollees in Medigap plans can shorten or avoid waiting periods for pre-existing conditions if they buy a Medigap policy during the Medigap open enrollment period, using it to replace their “Creditable coverage ” (Medigap).”
Applicants with a minimum of six months of continuous prior creditable coverage with another Medigap plan or provider usually won’t have to wait.
Many other types of private healthcare coverage also count towards Creditable Coverage for buying a Medigap policy.
However, the insurer will likely only count this prior coverage if it was continuous for a minimum of 63 days before applying for your new Medigap policy.
Can I Switch from Medicare Advantage to Medigap?
Yes. You can switch from Medicare Advantage policies to Medigap. You won’t have to undergo the medical underwriting process if you change within the first year of MA coverage.
However, it’s illegal for private insurers to sell you a Medigap policy while you’re still a member of a Medicare Advantage plan.
Guaranteed Issue Rights

You might qualify for “guaranteed issue rights,” such as the Medicare Advantage example we just covered.
With guaranteed issue rights, the Medigap insurer cannot reprimand your application to join its Medigap scheme with:
- higher premiums,
- denial of coverage,
- or a waiting period.
If your employer recently ended their healthcare coverage, you move to a different area of the US where your MA plan no longer offers you coverage, or your Medigap provider goes bankrupt, you qualify for a guaranteed issue right to a Medigap scheme of your choosing.
Frequently Asked Questions
When can Medicare Supplement Insurance Plans be purchased?
Medicare Supplement Insurance Plans, also known as Medigap plans, can generally be purchased during the Medigap Open Enrollment Period. This period begins on the first day of the month in which you turn 65 and are enrolled in Medicare Part B.
It lasts for six months and guarantees you the right to buy any Medigap plan available in your area without being denied or charged higher premiums due to pre-existing conditions.
Is there a specific time frame for enrolling in Medicare Supplement Insurance Plans?
Yes, the best time to enroll in a Medicare Supplement Insurance Plan is during the Medigap Open Enrollment Period. This is the six-month window that starts when you’re both 65 or older and enrolled in Medicare Part B.
During this period, insurance companies are required to offer you Medigap plans, regardless of your health condition, and they can’t charge higher premiums due to your health.
Can you enroll in Medicare Supplement plans at any time of the year?
While you can apply for a Medicare Supplement Insurance Plan at any time of the year, the Medigap Open Enrollment Period is considered the ideal time to do so. Applying during this period ensures you the most favorable terms, including coverage without medical underwriting and better premium rates.
What happens if I miss the Medigap Open Enrollment Period?
If you miss the Medigap Open Enrollment Period, you can still apply for a Medicare Supplement Insurance Plan at any time, but insurance companies may use medical underwriting to assess your health status.
This could lead to higher premiums or even denial of coverage based on your health conditions.
Can I change my Medicare Supplement plan after the enrollment period?
Yes, you can change your Medicare Supplement Insurance Plan after the enrollment period. However, if you decide to switch plans outside of the Medigap Open Enrollment Period, insurance companies may require medical underwriting, which could impact your premium rates and eligibility for coverage.
Are there any exceptions to the Medigap Open Enrollment Period?
Some states have additional enrollment periods or guaranteed issue rights that provide special circumstances for purchasing Medicare Supplement Insurance Plans outside of the standard Medigap Open Enrollment Period.
These could include situations like losing other health coverage or moving to a new state.
Can I apply for a Medicare Supplement plan if I’m under 65?
In most states, individuals under 65 who are eligible for Medicare due to disability may not have the same Medigap protections. However, some states require insurance companies to offer Medigap plans to individuals under 65. It’s important to check the regulations in your state.
Are Medicare Supplement plans the same as Medicare Advantage plans?
No, Medicare Supplement Insurance Plans (Medigap) and Medicare Advantage plans are different.
Medigap plans work alongside Original Medicare to cover certain out-of-pocket costs, while Medicare Advantage plans are an alternative way to receive Medicare benefits through private insurance companies, often including additional coverage like prescription drugs and dental.
Can I be denied a Medicare Supplement plan during the enrollment period?
No, during the Medigap Open Enrollment Period, insurance companies are generally not allowed to deny you a Medicare Supplement Insurance Plan based on your health status or pre-existing conditions. They must offer you any available Medigap plan, and they cannot charge higher premiums due to your health.
Do Medicare Supplement plans cover prescription drugs?
No, Medicare Supplement Insurance Plans do not cover prescription drugs. If you need coverage for prescription medications, you would need to enroll in a separate Medicare Part D prescription drug plan.
These plans are designed to work alongside Original Medicare and Medigap plans to provide prescription drug coverage.
When Can Medicare Supplement Insurance Plans Be Purchased
If you’re thinking about purchasing Medicare Supplement Insurance Plans, comparing rates from different insurers and for different plans is essential.
To get the process started, submit the form to the right or give us a call at 1-888-891-0229.
We’ll provide you with accurate quotes from the most reputable insurers in your area.
Updated December 4th, 2022


