Medigap
Medigap, also known as Medicare Supplement Insurance, is a supplemental health insurance policy offered to those who have signed up for Medicare.
This type of coverage is designed to help cover the costs not covered by traditional Medicare, such as copayments, coinsurance, and deductibles. It can also provide additional services not provided by Original Medicare such as coverage for emergency medical care while traveling abroad or at home in the US.

What is Medigap?
Medigap plans are private health insurance policies designed to work with other forms of Medicare coverage, like Part C and Part D plans.
Medigap covers many expenses that aren’t covered by original Medicare, like co-payments, coinsurance, and deductibles. One of the most important benefits of Medigap is that it can provide some financial protection if you need expensive treatments not covered by Original Medicare alone.
It can also help pay for some prescription drugs that would otherwise be excluded from your coverage under original Medicare or other types of health insurance.
Medigap plans come in different levels of coverage from basic to comprehensive depending on how much additional coverage you need. Generally speaking, higher levels of Medigap plans will generally cost more than basic ones but may offer better protection from out-of-pocket costs associated with healthcare services not covered under your primary plan.
In addition, it’s important to keep in mind that Medigap plans don’t replace your existing Medicare coverage; they simply supplement it.
 When choosing a Medigap plan, you should consider factors such as:
When choosing a Medigap plan, you should consider factors such as:
- your current level of coverage under existing health insurance policies,
- any pre-existing conditions you may have that are not covered by those policies,
- and what types of services are available through them (such as preventive care).
There’s also the matter of cost—since Medigap premiums vary greatly between companies and states—so it pays to compare different options before deciding on one provider or another.
Additionally, most people find that a combination of traditional government-backed programs like Medicaid or Medicare Advantage Plans (MAPs) combined with a Medigap policy provides a well-rounded package of financial protection in case serious health issues arise later in life down the road.
In summary, Medigap is an important supplemental health insurance policy designed to help fill gaps left by traditional types of medical insurance coverage such as Part C and Part D programs and private insurers alike.
Although these policies come at varying costs depending on the provider and state offering them, these plans are often found useful for those individuals seeking additional financial security against out-of-pocket medical expenses in the event their primary insurer does not cover them adequately enough or at all.
Who is Eligible for Medigap Insurance?
Medigap insurance, also known as Medicare Supplement Insurance, is designed to help cover the costs that Original Medicare does not.
It helps individuals with Medicare cover out-of-pocket expenses such as deductibles, copayments, and coinsurance for medical services. Medigap coverage is administered and sold by private insurance companies, so there are distinct differences between the different plans.
So who may enroll in Medigap insurance?
Individuals who are enrolled in both Part A and Part B of Medicare can apply for Medigap coverage. Additionally, applicants must be at least 65 years old or older to qualify for Medigap coverage; however, some states may offer Medigap plans to individuals under 65 with certain disabilities.
It’s important to note that while Medicare usually denies an individual’s application if they have a pre-existing condition or develop one after their enrollment date, Medigap insurers cannot deny someone due to a pre-existing health issue if they apply during their initial enrollment period.
This period is referred to as the six-month window when individuals first become eligible for Part B of Medicare and when they should consider applying for a Medigap plan. During this period, insurance companies must offer all applicants any plan they sell regardless of their current or past health status.
If you’re considering applying for a Medigap plan it’s best to do so during your open enrollment period as this guarantees your acceptance into any plan the insurer offers. After that six-month period ends though you may still be able to obtain coverage but will likely face restrictions based on your medical history and/or other factors such as age or location.
Furthermore, during this time your premium rates may be higher than what was offered during the open enrollment window due to potentially higher risk associated with issuing you a policy after that period expired.
Overall while it requires some research on your part it’s important to understand who is eligible for Medigap insurance in order to make sure you get the best possible coverage at the most affordable rate available given your specific circumstances.
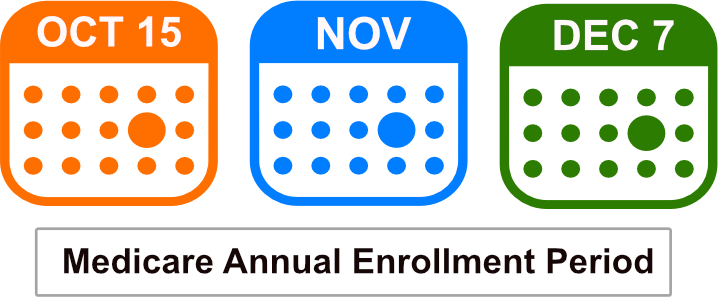
When can you enroll in a Medigap Plan?
Enrolling in a Medigap plan is an important step to take in order to ensure that your health care needs are covered. Medigap plans provide supplemental coverage of medical expenses not typically covered by Original Medicare, such as copayments, coinsurance, and deductibles.
As such, they’re an important part of any retirement plan that involves health care.
6-Month Medigap Open Enrollment Period
The good news is that there are several opportunities for you to enroll in a Medigap policy. One of the most popular times for enrollment is when you first become eligible for Medicare Part A or B (also known as original Medicare). This is generally when you turn 65 or if you have disability-related Medicare coverage.
During this initial enrollment period, insurance companies are required to offer Medigap coverage without taking into account pre-existing conditions, so it can be one of the best times to purchase a plan.
You may also be able to enroll during certain “guaranteed issue” periods, which occur after the initial enrollment period has passed. Generally speaking, this means that insurance companies must offer you a plan even if you have pre-existing conditions — as long as you join within 63 days after losing other creditable coverage (like employer-sponsored health insurance).
 Finally, some states may allow open enrollment periods where anyone can join a Medigap policy regardless of age or health status.
Finally, some states may allow open enrollment periods where anyone can join a Medigap policy regardless of age or health status.
These open enrollment periods usually last just a few months per year and vary by state.
It’s important to note that regardless of when and where you enroll in a Medigap policy, premiums may still be affected by your age and health condition.
However, during certain enrollment periods mentioned above, premium increases due to pre-existing conditions will be prohibited.
Overall, understanding when and how to enroll in a Medigap policy can be tricky — especially considering the complexities of modern healthcare policies and laws — but it’s an absolutely vital step for anyone who wants reliable financial protection against unexpected medical costs associated with Medicare Part A or B coverage gaps.
Knowing what opportunities exist for enrollment is key to making sure all your healthcare needs are covered throughout your retirement years!
Medigap Plans
Medigap plans are an important and often overlooked aspect of healthcare. Medigap plans are designed to help supplement the cost of regular Medicare by covering some or all of the out-of-pocket costs associated with medical care.
They are designed to help fill in the gaps that Medicare does not cover, such as copayments, coinsurance, and deductibles.
Medigap plans come in 10 different standardized varieties–lettered A through N–which have varying levels of coverage. Plans A, B, C, F, K, and L offer the most coverage; while Plans M and N offer more limited coverage.

Generally speaking, Plan F is the most comprehensive Medigap plan available; it covers all 8 major benefits listed by Medicare. It includes things like Part A coinsurance hospital costs up to 365 days after Medicare benefits have been used up as well as Part B coinsurance/copayments and emergency foreign travel exchange coverage.
It is important to note that Medigap plans do not cover long-term care or prescription drugs. Those must be covered with other supplemental insurance policies or a standalone Part D prescription drug plan. Additionally, Medigap policies must be purchased from a private insurer that is approved by Medicare.
In order to determine which type of Medigap plan is best for an individual’s needs, they should contact their local insurance company for more information about what type of policy would work best for them and how much it would cost.
It is also important to remember that even though these plans help cover some out-of-pocket expenses associated with medical care, individuals may still need to pay deductibles or co-pays depending on their particular plan’s coverage specifications.
Overall, Medigap plans can provide much-needed financial support when it comes to paying medical bills not covered by traditional Medicare components.
With 10 different standardized varieties ranging from very comprehensive (Plan F) to very limited (Plans M and N), there is sure to be one that meets every individual’s specific needs-from those who don’t require extensive coverage but still want something extra outside of traditional Medicare plans all the way up to those who need full coverage of out-of-pocket costs associated with medical care services covered under original Medicare parts A and B.
Medigap Plan F
Medigap Plan F is a supplementary insurance plan that provides coverage for Medicare beneficiaries’ out-of-pocket costs. This type of plan is designed to provide additional financial assistance so that individuals can afford their medical care without having to worry about paying large amounts out-of-pocket.
Plan F is a very popular plan because it covers 100% of the gaps of Medicare Part A and Part B. This means you pay nothing except for your monthly premium for all Medicare-approved expenses.
Medigap Plan F covers all expenses that Original Medicare does not, including copayments, coinsurance, and deductibles.
It is important to note that although Medigap Plan F covers many expenses, there are certain services it does not cover. These include long-term care, vision care, hearing aids, eyeglasses, dental care, and private-duty nursing.
Additionally, Medigap Plans do not cover prescription drugs. If you need coverage for these types of services or products you may want to consider enrolling in a Part D prescription drug plan or purchasing a separate policy.
Who can enroll in Medigap Plan F?
While Plan F does offer great coverage, it can be quite expensive and is only offered to those who were enrolled in Medicare prior to January 1st of 2020. Anyone new to Medicare may not enroll in Plan F, however, Medigap Plan G is likely a better option for most people anyway.
Another benefit of Medigap Plan F is that it provides access to an extensive network of healthcare providers including hospitals, doctors, and specialists who accept the plan. Additionally, this type of plan offers protection against any increases in cost due to inflation as premiums will remain constant regardless of how costs increase over time.
Furthermore, the beneficiary has the ability to choose his or her own doctor so they can receive quality care at their convenience.
Finally, Medigap Plan F offers security for those who cannot afford catastrophic medical bills and helps alleviate out-of-pocket costs associated with traditional Medicare plans.
For those looking for supplemental health insurance coverage, this plan may be an ideal choice as it covers many expenses not included under Original Medicare plans while also providing access to a wide network of healthcare providers at an affordable rate.
Medigap Plan G
Medigap Plan G is a unique and popular supplemental health insurance plan that helps cover any gaps in Original Medicare coverage. This plan helps to complement the basic benefits of Medicare, making it easier for individuals to access the care they need for their health and well-being.
One of the main benefits of Medigap Plan G is its very extensive coverage, providing protection against financial risk associated with high medical costs in many areas.

It covers all deductibles, copayment amounts, and coinsurance amounts not covered by Original Medicare Parts A and B except for the Medicare Part B deductible. This averages around $230 per year.
Coverage with Medigap Plan G includes hospital costs up to an additional 365 days after Medicare benefits have been exhausted and certain preventive care services like annual wellness visits at no cost. It also offers coverage for three pints of blood every year as part of transfusions and other medical treatments.
Plan G also covers skilled nursing care and foreign travel emergencies, two services not covered under Original Medicare. It can help pay for Part B excess charges (costs exceeding those set by Medicare), as well as the Part A hospice coinsurance amount that original Medicare does not cover.
In terms of costs, Medigap Plan G premiums vary from one insurer to another, depending on a variety of factors including location, age, gender, and smoking status. Most people pay a monthly premium for this policy; however, some states may offer discounts if more than one person is enrolled in the same policy or if discount programs are available from participating insurers.
Additionally, since this plan is regulated by federal laws governing private insurers, there are certain restrictions on rate increases that can be imposed over time without prior approval from state regulators.
Overall, Medigap Plan G provides comprehensive coverage at relatively affordable prices when compared to other types of supplemental insurance plans.
By taking into account all potential out-of-pocket expenses associated with Original Medicare coverage – including deductibles and copayments – individuals can rest assured that they will have access to quality medical care when needed without incurring excessive financial burden upon themselves or their families.
Medigap Plan N
Medigap Plan N is a very popular supplemental health insurance plan offered by private insurers to Medicare beneficiaries that helps cover the gaps in traditional Medicare coverage, though it’s slightly different than Medigap Plan G.
Under the Medigap Plan N, enrollees will be able to have access to some of the same basic benefits as with other Medigap plans.

These include coverage for coinsurance and copays for hospitalizations and skilled nursing care, as well as medical services such as emergency room visits and outpatient surgeries. However, there are some differences between Medigap Plan N and other Medigap plans.
For example, under this plan, enrollees will be responsible for paying up to $20 when they visit their doctor or go to the emergency room after the Medicare Part B deductible is met each year. This contrasts with some of the other Medigap plans which cover those costs in full.
Medicare Plan N Cost
In terms of cost, premiums may differ depending on where you live and which insurer you choose. Generally speaking, however, premiums tend to be slightly lower than those associated with more comprehensive Medigap plans like Plans F or G.
The total out-of-pocket costs associated with Plan N may also end up being lower than those associated with other plans since enrollees will have higher copayments than would otherwise be required in more comprehensive plans.
Overall, the main benefit provided by Medigap Plan N is that it helps bridge the gap between what traditional Medicare covers and what medical expenses must still be paid out-of-pocket by enrollees themselves.
It provides basic coverage for hospitalizations and medical services such as emergency room visits while also offering lower premiums than most other supplemental health insurance policies offer – making it an attractive option for people looking to save money while also receiving a measure of financial protection against unexpected healthcare costs down the road.
Medigap vs Medicare Advantage
Medicare and Medigap insurance are two types of health insurance plans. Medicare is a federal health insurance program for people over 65, while Medigap is an additional policy that covers the costs not covered by Medicare (like deductibles and copayments). Medigap works alongside Medicare and Medicare Parts A and B are your primary insurance.
Original Medicare covers 80% of your hospital stay costs after a deductible has been met; however, most people need help to cover the remaining 20%. A Medigap plan can help pay for this remaining balance when you receive medical care from doctors who accept original medicare assignment fees – meaning they accept payment from medicare as full payment towards their services rendered.
A Medicare Advantage plan is a type of private health insurance plan that provides more coverage than just traditional Medicare. It often includes additional benefits such as vision, dental, hearing aid services, or prescription drugs.
Medicare Advantage plans are different from both Original Medicare and Medigap plans. Medicare Advantage plans are offered by private companies approved by Medicare and provide all your Part A (hospital) and Part B (medical) coverage in one plan.
Most of these plans also offer additional benefits that Original Medicare or Medigap do not cover, such as routine vision or dental care, prescription drug coverage, or even hearing aids at no extra cost to you.

The main difference between Medigap and a Medicare Advantage plan is in what each covers. With Medigap policies, you can choose from 10 different plans to cover specific areas like hospital stays or doctor visits. These policies do not provide extra benefits such as vision care or dental coverage.
A Medicare Advantage plan allows you to get more comprehensive coverage than just traditional Medicare does by offering additional benefits such as vision care and prescription drug coverage. You may also be able to get added features like wellness programs or gym memberships with a Medicare Advantage plan – something not available with Medigap policies.
However, these plans still have extra out-of-pocket expenses as well as networks that you may have to stay within. Medigap policies do not have networks and may be used anywhere in the country with any provider that accepts Medicare.
Frequently Asked Questions
What is Medigap and how does it work?
Medigap, also known as Medicare Supplement Insurance, is a type of private health insurance that helps cover the gaps in Medicare coverage. It pays for certain out-of-pocket costs such as deductibles, copayments, and coinsurance.
Who is eligible for Medigap coverage?
In most states, individuals who are 65 years or older and enrolled in Medicare Part A and Part B are eligible to purchase a Medigap policy. Some states have additional eligibility criteria for Medigap coverage.
Can I buy a Medigap policy if I have a pre-existing condition?
Yes, you can generally purchase a Medigap policy even if you have a pre-existing condition. However, depending on your state and the timing of your enrollment, you may face a waiting period before the policy covers your pre-existing condition.
How do I choose the right Medigap plan for me?
The right Medigap plan depends on your individual needs and preferences. Consider factors such as your budget, health condition, and the level of coverage you desire. Compare different plans offered in your area to find the one that best fits your requirements.
Are Medigap plans standardized?
Yes, Medigap plans are standardized in most states. This means that each lettered plan (e.g., Plan A, Plan B) offers the same basic benefits, regardless of the insurance company selling it. However, premiums may vary between insurance companies.
Can I switch Medigap plans?
Yes, in most cases, you can switch Medigap plans. However, you may need to go through medical underwriting, and your acceptance into a new plan may depend on your health condition at the time of application.
Will Medigap cover prescription drugs?
No, Medigap plans do not cover prescription drugs. If you need coverage for prescription medications, you will need to enroll in a separate Medicare Part D prescription drug plan.
Are there any Medigap plans for those under 65 with disabilities?
Some states offer Medigap plans to individuals under 65 with disabilities. However, availability and eligibility criteria may vary, so it is essential to check with your state’s insurance department for more information.
Can I use my Medigap plan outside of the United States?
Most Medigap plans do not provide coverage for medical services received outside of the United States. However, some plans may offer limited coverage for emergencies during foreign travel. It is advisable to check your plan’s coverage details.
How much does a Medigap policy cost?
The cost of a Medigap policy varies depending on factors such as your age, location, and the specific plan you choose. Generally, you pay a monthly premium in addition to your Medicare Part B premium. Comparing prices from different insurance companies is recommended to find an affordable option.
Where can I buy a Medigap Policy?
When it comes to shopping for a Medigap policy, you have a wide array of choices at your disposal.
While many may lean towards searching for nearby agents or brokers, it is important to note that the best deals often come from a website like ours.
Here you can shop for Medigap plans and view the rates for each plan in your area from the top insurance companies. And if you try to call each company directly to get their rates, you will end up having to talk to multiple salespeople, all trying to sell you their policy without telling you the rates from other companies.
Remember, each company offers the same identical coverage and Medigap plans, but they all charge different rates!
Fortunately, our team is equipped to handle the hard part for you, for FREE. And we’ll check your rate each year to make sure you’re always paying the least amount possible for your coverage.
To get started, just give us a call today at 1-888-891-0229.
Updated December 4th, 2022

